Cervical screening pilot for trans patients could revolutionise healthcare and save lives
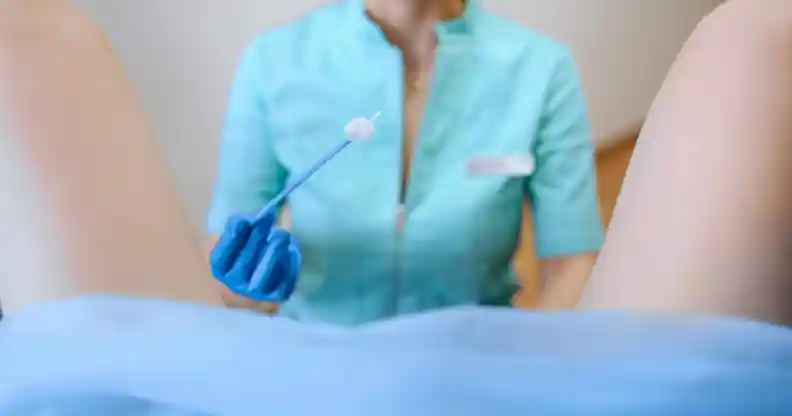
Cervical screenings are vital for every person with a cervix, regardless of gender. (Envato)
A UK cervical screening pilot programme for trans men and non-binary people was so successful it could be used as a model for programmes around the world.
The pilot programme was launched in October 2019 in conjunction with the NHS as part of a study to address cervical cancer in trans and non-binary communities.
It offered weekly cervical screening clinics, only staffed by healthcare professionals with experience in treating trans and non-binary patients.
Of those who attended the clinic and gave feedback, 100 per cent were satisfied with the service, and a majority (60 per cent), said they would not have been screened if it were not for the clinic.
In the UK, screening is recommended every three years for all people with a cervix between the ages of 25 and 49, and every five years for those between age 49 and 64.
But trans and non-binary people with cervixes are often left out of guidance, or avoid attending screenings for fear of discrimination and misgendering.
“Trans men and non-binary people are often reluctant to receive cervical screening, raising their risk of undetected human papillomavirus [HPV], which could lead to cervical cancer,” said Alison May Berner, a specialty trainee and clinical research fellow in medical oncology at Barts Cancer Institute in London, a specialist registrar with the Tavistock and Portman Gender Identity Clinic and the study’s lead author, per News Medical.
The results of the study were presented at the American Association for Cancer Research’s Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved this month, indicating that it could have international implications, and Berner said she wants further research to look at trans-specific cervical screenings in a GP setting.
She said: “People assume that this population’s health care-related needs are solely related to transition. That’s not true.
“Trans and non-binary people are at risk of HPV infection and cervical cancer if they continue to retain a cervix, and they stand to benefit from programs designed specifically for them.
“If you’re a trans or non-binary person living in a place where these specialist services do not exist, I would encourage you to work with a trusted health care professional to build relationships and ensure that you get the appropriate screenings, while continuing to have your identity respected.”

