New Zealand to introduce PrEP for less than two dollars a month
New Zealand has announced that it will publicly fund PrEP (Pre-Exposure Prophylaxis) for just $1.20 a month for a prescription.
The country is one of a few that have made the decision to make the HIV prevention medication available at a reduced price.

Pre-Exposure Prophylaxis (PrEP)
Related: A once-a-week HIV pill could soon be available
From March 1st, the treatment will be rolled out to those who are most at risk of contracting HIV.
Previously, a prescription for the drug would cost US$731 a month, meaning that many users would import the medication.
However, getting it from overseas would still cost around US$36 a month.
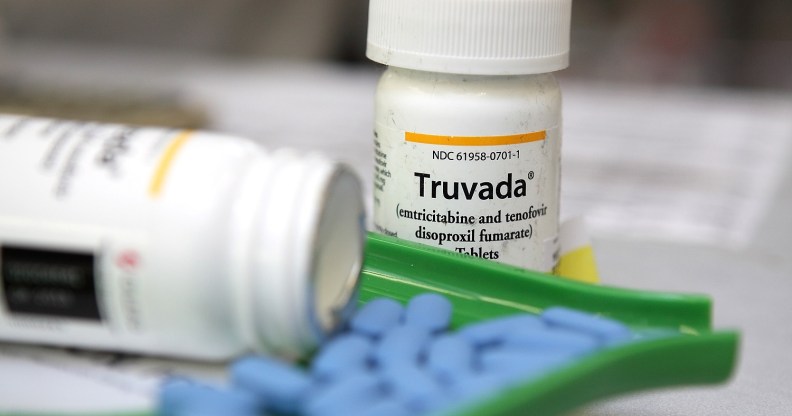
By publicly funding Truvada, the cost of a quarterly prescription will fall to just US$3.60, which works out to $1.20 a month making it cheaper than in almost any other country in the world.

PrEP
Related: What is bareback sex and what do I need to know about it?
PrEP is up to 99% effective at preventing HIV transmission.
The decision to publicly fund the preventative drug has been celebrated by LGBTQ and HIV/AIDS activists across the country.
The executive director of New Zealand AIDS Foundation (NZAF), Dr Jason Myers, said that it will have an incredibly positive impact on the rate of HIV transmission.
“Providing adorable access to PrEP for those who need it will make an enormous difference to those most at risk of HIV transmissions.
“It’s a giant leap forward for our ambitious goal of ending new HIV transmissions in New Zealand by 2025.

Related: What is PrEP and how can I get it? Everything you need to know about HIV-preventing drugs
“For those who struggle with consistent condom use – which can be for a range of legitimate reasons – NZAF is delighted that there will now be publicly funded access to this effective, alternative way of staying safe from HIV for those who need it,” he added.
The government agency that rules on which pharmaceuticals to publicly fund, PHARMAC, announced that it would be publicly funding PrEP in November 2017.
PrEP will be available to men who have sex with men, transgender people, people recently diagnosed with another STI, infrequent users of condoms and people in a relationship with an HIV-positive person.
In 2016 New Zealand recorded its highest number of new HIV diagnoses since the AIDS crisis began in the 1980s.

HIV testing kits are available at doctors surgeries (Photo by: BSIP/UIG via Getty Images)
The number of new diagnoses was up for another year, with the vast majority of those affected men who have sex with men.
Myers added that PHARMAC’s decision to follow advice from NZAF to include trans men as being eligible to access the subsidized PrEP was “very important step in addressing one of the health inequalities faced by trans men.”
“We are also extremely heartened to see that PHARMAC took on board suggestions to expand funded PrEP access to include transgender men who are at high risk of HIV,” he said.
Other countries to subsidize PrEP are Brazil, France, Norway, Brazil, Belgium and Scotland.
The World Health Organisation strongly backed the use of PrEP as HIV prevention in 2014, but global provision remains patchy.
In England, PrEP is now available on the NHS to at-risk groups including gay men for free as part of a three-year trial.
NHS England is investing £10 million in the trial. Privately, generic PrEP drugs are available for around £39 a month.
The cost of a public PrEP scheme is currently higher than buying the drugs privately, as Gilead still holds patents covering the provision. Branded Truvada costs £350 a month, and the cost of public PrEP schemes are projected to plummet once Gilead’s patents expire.
HIV researchers believe rolling out PrEP might actually be cost-effective in the long term.
As the lifetime cost of treating just one HIV infection can be up to £380,000, a PrEP scheme would only need to prevent a handful of transmissions in order to be cost-effective.

