HIV life expectancy now nearly the same as general population

People who visited the spa are being asked to get tested for blood-borne infections (Getty)
Young people with HIV now have a practically normal life expectancy, new research has revealed.
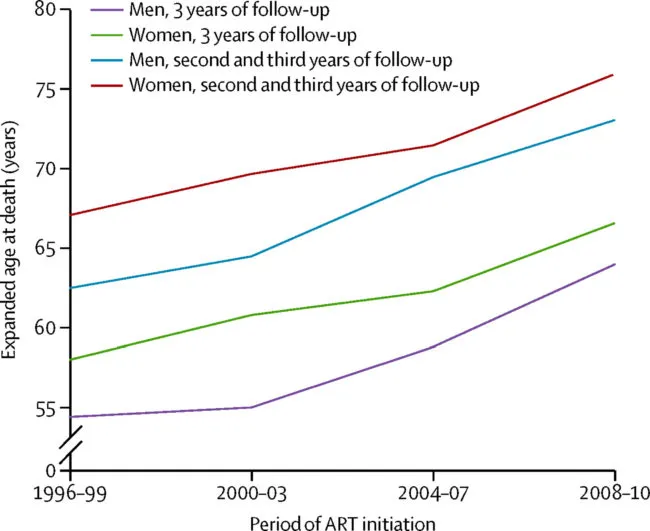
The expected age at death of a 20-year-old patient starting antiretroviral therapy (ART) between 2008 and 2010 before the disease had fully taken hold was 78 years old.
Life expectancy in the US is 78.9 in the US and 80.1 in the UK.
The 17-year government-funded study published today in The Lancet was conducted on more than 88,000 people over the age of 16.
It showed that between 1996 and 2010, life expectancy in 20-year-old patients beginning ART increased by about 9 years in women and 10 years in men.
The increase in life expectancy was down to rapid improvements made in treatment, the study’s authors said, commenting that HIV healthcare had “improved substantially in the past two decades”.
Prof Helen Stokes-Lampard, who chairs the Royal College of GPs, told the BBC: “It’s a tremendous medical achievement that an infection that once had such a terrible prognosis is now so manageable, and that patients with HIV are living significantly longer.
“We hope the results of this study go a long way to finally removing any remaining stigma associated with HIV,” she continued.
This, in turn, would mean “ensuring that patients with HIV can live long and healthy lives without experiencing difficulties in gaining employment and – in countries where it is necessary – obtaining medical insurance.”
She added that steps were being taken to increase appropriate HIV testing by GPs.
The study followed news last week that scientists have cured living animals of HIV for the first time.
Starting treatment early is crucial to increasing your life expectancy, emphasised the experts behind the study, known as Bristol University’s Antiretroviral Therapy Cohort Collaboration.
ART involves a combination of three or more drugs to block the usual advance of HIV.
And the study’s authors said the latest developments in the field meant newer drugs have fewer side effects and are better at preventing the virus from spreading.
The virus is also less likely to build up a resistance to these drugs.
And improved screening and prevention programmes, in conjunction with more awareness and treatment of the health issues caused by HIV, have helped as well.
Around one in eight people are still unaware that they have the virus, a deficit which doctors say must be fixed to ensure this crucial treatment is carried out.
Mental health issues are prominent among people with HIV, with a study last month finding that HIV-positive men are twice as likely to die by suicide than the general population.
More than 100,000 people are living with HIV in Britain.
There have been ongoing legal battles around the funding of PrEP, a drug that can reduce the risk of being infected with HIV by up to 86% if taken daily.
It has been endorsed by the World Health Organisation and Centers for Disease Control and Prevention for at-risk men who have sex with men (MSM).
NHS Wales has agreed to trial fund the drug, along with NHS Scotland who announced plans earlier this year.
NHS England is also due to trial the drug following Scotland’s lead.

